How Real-Time Alerts in an eMAR System Prevent Missed Doses and Errors (2025 Guide)
Real-time alerts have quietly become one of the most practical safety nets in modern medication management in nursing. Missed doses, late administrations, or duplicate entries rarely come from bad practice; they’re usually the product of busy shifts, complex regimens, last‑minute prescription changes, or interruptions at the trolley. The truth is, a strong medication administration policy backed by an intelligent eMAR system gives teams the prompt they need at the exact moment they need it.
At eMAR Plus, we see this every day. Homes that embed alerts into their workflows reduce avoidable risk, spend less time chasing paperwork, and walk into inspections with confidence. In this 2025 guide, we unpack how real-time alerts work, why they matter, and how to implement them without creating “noise” for your team.
Why Missed Doses and Errors Still Happen
Even with clear procedures, the day-to-day reality is challenging:
Interrupted rounds: Phone calls, questions, or resident needs break concentration.
Complex schedules: Polypharmacy and variable timings increase cognitive load.
Shift handovers: Information gaps at changeover can lead to omissions or double‑dosing.
Agency staff: New starters may not know the local routine or chart layout.
Paper dependence: Illegible handwriting, misplaced MAR sheets, and delayed updates make it hard to spot risk in time.
A robust medication administration policy sets the expectation. An eMAR system with real‑time alerts turns that policy into a living safety mechanism at the bedside.
What Do We Mean By “Real-Time Alerts”?
In the context of medication administration software, real-time alerts are automated prompts triggered by medication schedules, clinical rules, or workflow events. Typical alert types include:
Due / overdue dose alerts: Remind staff when a medicine is approaching or has passed the scheduled time.
Duplicate dose prevention: Flag if a dose has already been given or if the safe window hasn’t elapsed (especially for PRN medicines).
Timing window checks: Enforce safe intervals for time-sensitive drugs.
Change notifications: Surface pharmacy updates (new starts, stops, dose changes) immediately, reducing transcription risk.
Stock and ordering prompts: Warn when supplies are low so a missed dose isn’t caused by stock-outs.
Escalation prompts: Nudge senior review when repeated deferrals or refusals occur.
Handled well, alerts don’t replace clinical judgement; they support it. They act as a second pair of eyes that never get tired.
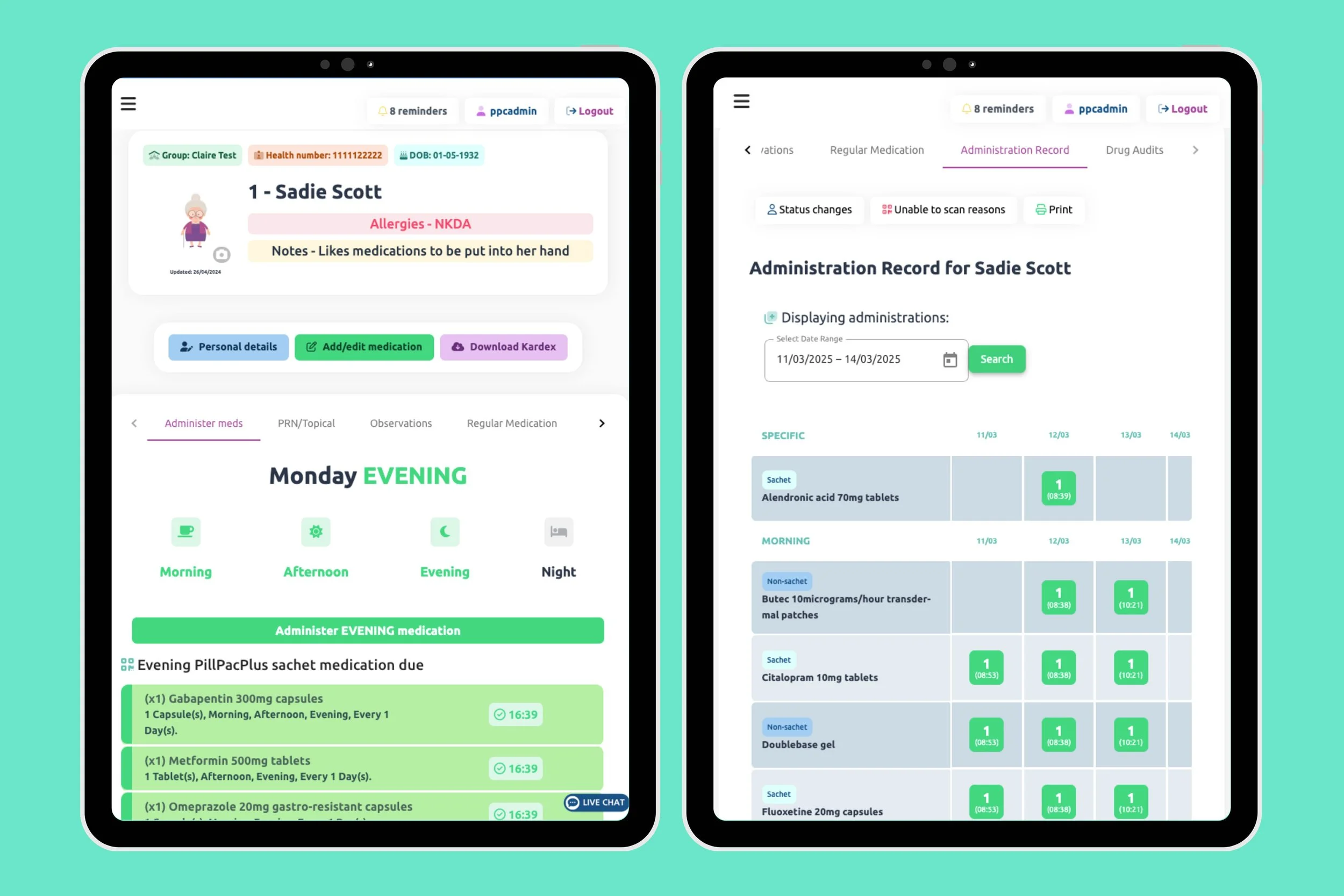
How & Where Alerts Work in eMAR Plus
eMAR Plus builds safety checks into the flow of work, so prompts appear exactly where clinicians make decisions. This section maps where each alert shows and why it reduces risk, making your medication administration policy and nursing care plan for medication management easier to deliver and evidence.
Medication round view (at the trolley): Clear due/overdue badges and timers surface priorities in real time, reducing reliance on memory during busy periods. These rules are configurable to match your policy’s grace windows, supporting safer medication management in nursing.
Resident MAR screen (point of care): PRN interval checks, duplicate‑dose prevention, timing‑window warnings and route/time mismatch prompts guide safe decisions, embedded in the eMAR system rather than added as extra steps.
Change log & pharmacy updates: Starts, stops and dose edits appear immediately to cut transcription risk. With PillPacPlus pouch scanning, point‑of‑administration barcode verification adds another barrier against selection errors.
Stock & ordering panel: Low‑stock and expiry alerts prevent omissions caused by supply issues, aligning stock management with your medication administration software workflows.
Manager dashboard & reports: Exception lists for missed/overdue doses, trends by unit/shift, and time‑stamped audit trails support governance, inspection readiness and accountability.
Put simply, the medication management software guides the round, and the alerts keep it honest, turning policy into day‑to‑day practice.
“The system’s real‑time alerts have helped prevent medication errors by notifying us if a dose is missed, or administered incorrectly… ensuring every resident receives their medication on time and exactly as prescribed.” Residential Manager, Hutchinson Care Homes
Alerts and UK Regulatory Expectations
Regulators don’t mandate specific software, but they do expect safe, consistent processes and complete, auditable records. CQC guidance and NICE recommendations emphasise accurate record‑keeping, the “five rights”, and timely administration. Real‑time alerting directly supports these outcomes by helping teams administer the right medicine, at the right dose, via the right route, to the right person, at the right time and record it accurately.
Read more: CQC guidance on electronic MARs (useful for understanding what inspectors look for).
Read more: NICE SC1: Managing medicines in care homes.
Alerts aren’t a shortcut to compliance, but they make it considerably easier for managers to demonstrate that the medication administration policy is embedded in daily practice.
Practical Scenarios Where Alerts Prevent Harm
Insulin and meal‑time coordination: Alerts matched to mealtime windows prompt staff if insulin is due but hasn’t been recorded, or if a resident didn’t eat, triggering a check of the care plan before proceeding.
Anticoagulant timing: For medicines with narrow therapeutic windows, alerts reinforce consistent timing and highlight omissions promptly, allowing timely escalation to the prescriber.
PRN analgesia: Real‑time prompts prevent early redosing and nudge staff to record efficacy, which closes the loop on symptom management and informs the next decision.
Antibiotic courses: End‑date alerts help ensure courses are completed and not continued inadvertently, preventing both missed doses and unnecessary extensions.
Controlled drugs: Prompts for witness checks and documentation ensures that legal requirements are met without slowing the round to a crawl.
Ready to Strengthen your Medication Safety Net?
If you’re reviewing your medication management in nursing pathways for 2025, it’s a good moment to combine a clear medication administration policy with a well‑configured eMAR system. Real‑time alerts won’t make decisions for you but they will ensure the right information reaches the right person at the right time.
See how eMAR Plus supports safer, quicker rounds with intelligent alerting and streamlined documentation.
Explore eMAR Plus features: https://www.emarplus.com/features
Talk to our team: https://www.emarplus.com/get-in-touch
This guide is for informational purposes and does not replace professional medical or regulatory advice.